Abstract
The importance of vital signs monitoring is no longer just a concern for healthcare professionals, but for patients as well. Many wearables with vital sign measuring capability are not accurate enough for the medical community. This article discusses the shortcomings of current measurement solutions and introduces a highly integrated healthcare sensor AFE.
Introduction
The importance of physiological vital signs as indicators of human health has long been understood by medical professionals, but the COVID-19 pandemic also heightened public awareness of their significance. Unfortunately, most people who find themselves undergoing continuous vital signs monitoring are likely already in a clinical setting being treated for an acute condition. Instead of using vital signs as an indicator for the effectiveness of disease treatment and patient recovery, the model for future healthcare will be to employ continuous and remote vital signs monitoring as a tool to identify potential indicators of disease onset, allowing interventions to take place by clinicians at the earliest opportunity before serious illness develops. It is envisaged that ever increasing integration of clinical-grade sensors will eventually enable the development of disposable, wearable vital signs health patches that can be replaced periodically (like contact lenses).

While many health and fitness wearables include vital signs measurement functions, the integrity of their readings can be questionable for several reasons, including the quality of sensors used (most are not clinical grade), the location at which they are mounted, and the quality of body contact while worn. Although these devices are sufficient to satisfy the desire for casual self-observation by nonhealth professionals using one convenient and comfortable wearable, they do not meet the standards of performance and accuracy required for trained medical professionals to properly assess the health of an individual and make an informed diagnosis. On the other hand, devices currently used to provide clinical-grade vital signs observation over extended time intervals can be bulky and uncomfortable, with varying degrees of portability. This article reviews the clinical significance of four vital sign measurements—blood oxygen saturation (SpO2), heart rate (HR), electrocardiogram (ECG), and respiration rate (RR)—and consider the best type of sensor to provide clinical-grade readings of each. A highly integrated healthcare sensor AFE combines the functions of three separate biosensors into a single package. This has the potential to bring much closer the concept of the wearable, disposable vital signs health patch.
Blood Oxygen Saturation
Healthy individuals typically have a blood oxygen saturation level in the region of 95% to 100%. However, levels of 93% or lower for SpO2 can be an indication that an individual is experiencing respiratory distress, making it an important vital sign for medical professionals to monitor regularly. Photoplethysmography (PPG) is an optical measurement technique that uses several LED transmitters to illuminate blood vessels under the surface of the skin and photodiode receivers to detect the reflected light signal, thereby allowing SpO2 to be calculated. While it has become a common feature in many wrist-worn wearables, PPG light signals are prone to interference from motion artifacts and transient variations in ambient lighting that can potentially cause spurious readings, meaning these devices do not provide clinical-grade measurements. In a clinical setting, SpO2 is measured using a finger-worn pulse oximeter (Figure 2) usually continuously attached to the finger of a stationary patient. While battery-powered, portable versions exist, they are only practical for making intermittent measurements.

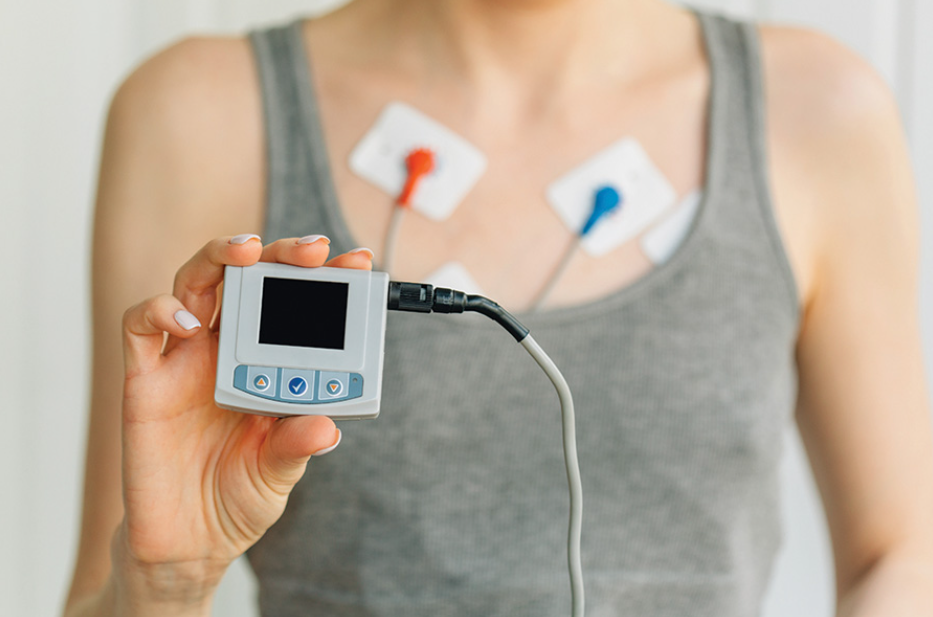
HR and ECG
A healthy HR is usually considered to be in the range of 60 to 100 beats per minute; however, the time interval between individual beats is not constant. Often referred to as heart rate variability (HRV), this means that HR is an average value measured over several beat cycles. In a healthy individual, HR and pulse rate are almost identical because blood is pumped around the body with each contraction of the heart muscle. However, some serious cardiac conditions can cause the HR and pulse rate to differ. For example, in the case of cardiac arrhythmias such as atrial fibrillation (Afib), not every muscle contraction within the heart pumps blood around the body—instead blood can accumulate within the chambers of the heart itself, a potentially life-threatening occurrence. Afib can be difficult to detect as it sometimes occurs intermittently and only for short transient intervals. The importance of being able to detect and treat this condition is evidenced by the fact that, according to the World Health Organization, one-quarter of all strokes in people over the age of 40 are caused by Afib.1 Since PPG sensors make optical measurements on the assumption that HR is identical to pulse rate, they cannot be relied on to detect Afib. This requires the electrical activity of the heart to be continuously recorded over an extended interval—the graphical representation of the heart’s electrical signal is called an ECG. The Holter monitor (Figure 3) is the most common clinical-grade portable device for this purpose. While these use fewer electrodes than static ECG monitors used in clinical settings, they can be somewhat cumbersome and uncomfortable to wear, particularly when sleeping.
Respiration Rate
The expected RR for most healthy people is 12 to 20 breaths per minute. An RR exceeding 30 breaths per minute may be an indicator of respiratory distress caused by a fever or some other reason. While some wearables solutions deduce RR using accelerometer or PPG techniques, clinical-grade measurement of RR is performed either by using the information contained in an ECG signal or by using a bioimpedance (BioZ) sensor that characterizes the electrical impedance of the skin using two or more electrodes attached to the body of a patient. While FDA-approved ECG functionality is available in some high end health and fitness wearables, bioimpedance sensing is a feature that is typically not provided as it requires the inclusion of a separate BioZ sensor IC. Apart from RR, BioZ sensors also enable bioelectrical impedance analysis (BIA) and bioelectrical impedance spectroscopy (BIS), both used in the measurement of body muscle, fat, and water composition levels. BioZ sensors also enable impedance cardiography (ICG) and are used to measure galvanic skin response (GSR), which can be a useful indicator of stress.
3-in-1 Sensor Solution
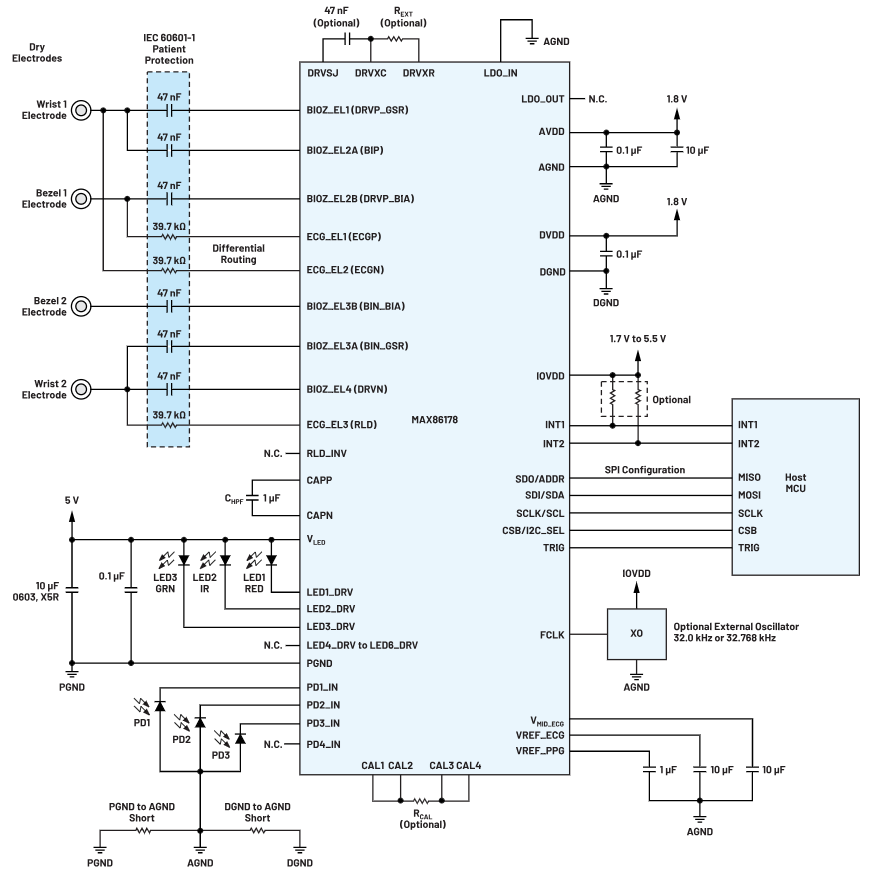
The functional block diagram of a clinical-grade vital signs AFE IC that integrates the functions of three separate sensors—PPG, ECG, and BioZ—into a single package is presented in Figure 4.
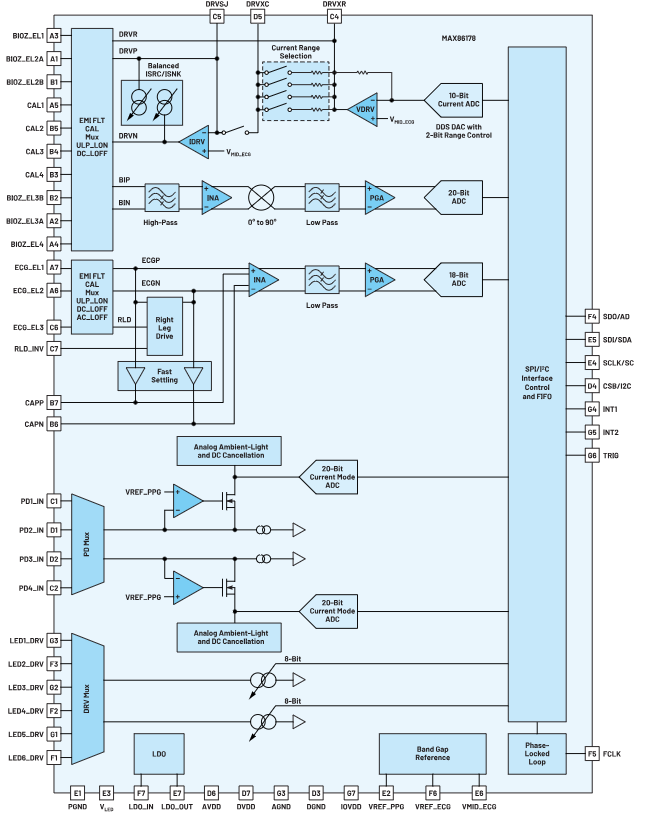
Its dual-channel PPG optical data acquisition system supports up to six LEDs and four photodiode inputs with the LEDs being programmable from two high current, 8-bit LED drivers. The receive path has two low noise, high resolution readout channels that each include independent 20-bit ADCs and an ambient light cancellation circuit, providing in excess of 90 dB of ambient rejection at 120 Hz. The PPG channel exhibits up to 113 dB SNR that supports SpO2 measurements at only 16 µA.
The ECG channel is a complete signal chain that provides all of the critical features necessary to collect high quality ECG data such as flexible gain, critical filtering, low noise, high input impedance, and multiple lead-biasing options. Additional features, such as fast recovery, AC and DC lead-off detection, ultra low power lead-on detection, and right leg drive, enable robust operation in demanding applications such as wrist-worn devices with dry electrodes. The analog-signal chain drives an 18-bit sigma-delta ADC with a wide range of user-selected output sample rates.
The BioZ receive channel has EMI filtering and extensive calibration features. It also has high input impedance, low noise, programmable gain, low-pass and high-pass filter options, and a high resolution ADC. There are several modes for generating input stimulus: balanced squarewave source/sink current, sinewave current, and both sinewave and squarewave voltage stimuli. A wide range of stimulus magnitudes and frequencies is available. It also supports BIA, BIS, ICG, and GSR applications.
FIFO timing data allows all three sensor channels to be synchronized. This AFE IC is available in a 7 mm × 7 mm 49-ball wafer-level package (WLP) with package dimensions of only 2.6 mm × 2.8 mm, making it ideal to be designed into, for example, a clinical-grade wearable chest patch (Figure 5).
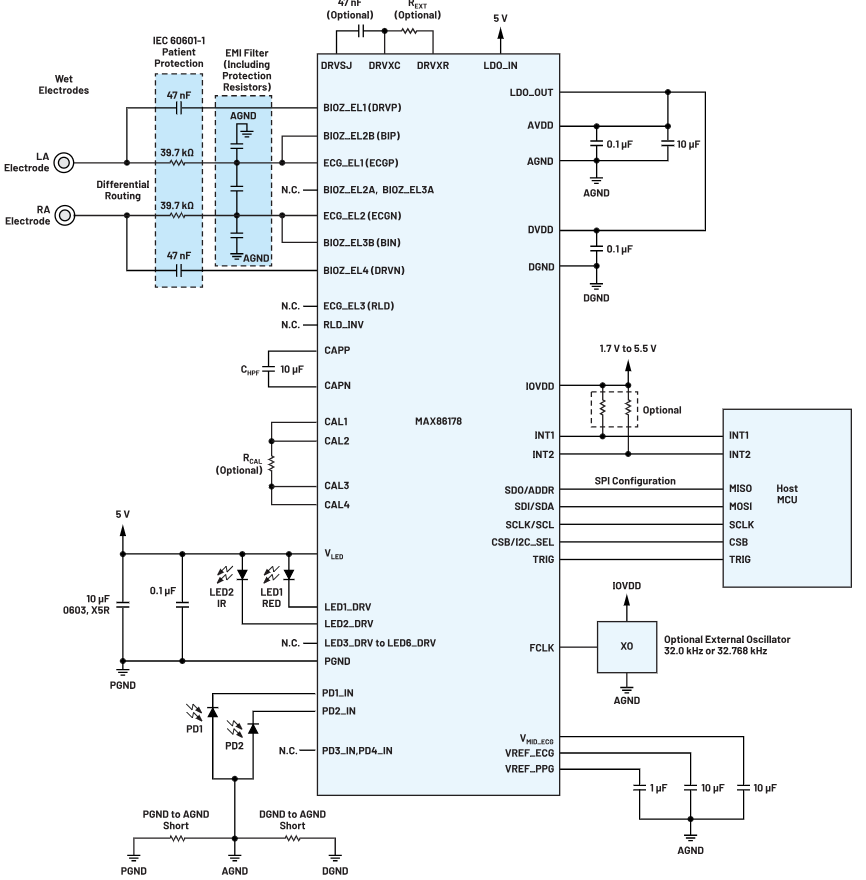
Figure 6 illustrates how this AFE can be designed into a wrist-worn wearable to provide on-demand BIA and ECG with continuous HR, SpO2, and electrodermal activity (EDA)/GSR.
Conclusion
SpO2, HR, ECG, and RR are important vital sign measurements that healthcare professionals use for diagnostic purposes. Continuous vital sign monitoring using wearable devices will be a key component in the model for future healthcare, allowing disease onset to be anticipated before symptoms develop. The measurements produced by many currently available vital sign monitors cannot be used by healthcare professionals because they use sensors that are not clinical grade while others simply do not have the capability to accurately measure RR because they do not include a BioZ sensor. This article presented an IC that integrates three clinical-grade sensors—PPG, ECG, and BioZ into a single package and showed how it can be designed into chest and wrist-worn wearables to measure SpO2, HR, ECG, and RR while also providing additional useful health-related features including BIA, BIS, GSR, and ICG. Apart from application in clinical-grade wearable devices, this IC is also ideal for integration into smart clothing to provide the type of information required by high performance athletes.